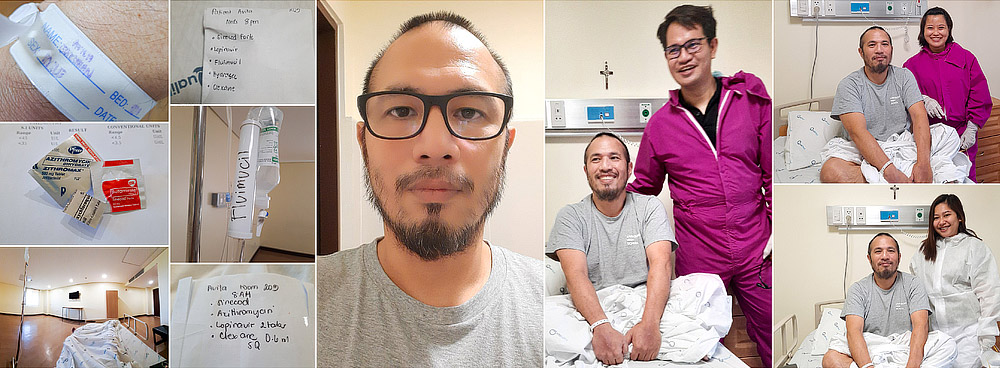
Many in the industry knows him as misterkodaker and he is one of the Philippines’ masters that I personally look up to. I am still stunned learning that he had been diagnosed with the Covid-19 virus. He was my photography teacher way back 2006 and I have so much respect on him as a mentor. I praise God for his speedy recovery.
Sharing with you the story of his battle here:
It was around 2 am on March 16, 2020 when I found myself outside the ER of a hospital near my Antipolo residence. It was the second day of the Metro-wide community quarantine.
I explained that I had been suffering from diarrhea the past two days and vomited prior to proceeding the hospital.
While in the ER, they took a stool sample, hooked me up to an IV and allowed me to sleep for two hours.
Since the results of the stool sample showed no trace of bacteria, I was prescribed medicine and oral rehydration salts and sent home.
On March 22, 2020 I was back in the ER. I still had diarrhea. The ER doctor took note that I was coughing and had a cold. The decision was made that I should be admitted as a PUI.
Unfortunately, the hospital could not accommodate me since 20 of their nurses were under quarantine. My wife and I started to think of other hospitals where I could be admitted. Antipolo and Metro Manila hospitals were already at full capacity.
At this point, my dad and elder brother had been informed about my situation. With their help, arrangements had been made for an ambulance to pick me up at home and bring me to Qualimed in Sta. Rosa, Laguna.
As soon as we arrived in Qualimed, I was wheeled straight into an isolation room.
Blood samples, nasal and throat swabs were also taken from me immediately thereafter.
They attached an IV to my left hand, wheeled an X-ray machine into my room and took and X-ray of my chest area. It was the first day and I was left amazed at the efficiency of the hospital staff.
On March 24, 2020, a CT scan of my lungs was taken to confirm the x-ray results that I did have pneumonia. This was also the day that I met one of my doctors for the first time, Dr. Pasayan, an infectious disease specialist.
He explained to me about my symptoms and how he suspected that I was Covid-19 positive based on my symptoms. Dr. Pasayan sought my consent to proceed with the treatment based on the assumption that I had Covid-19 even if the results of the swab test had not been returned yet.
He reasoned early intervention is key to successfully treating Covid-19. If the results come back negative, then the treatment would be stopped and nothing would have been lost.
He explained that one of the medicines that I will be taking was an anti-malarial drug which can cause an erratic heartbeat. Therefore, to ensure that It could be safe for my heart, an ECG had been taken earlier.
(This antimalarial drug would later become unavailable and I was eventually switched to a medicine that is used to treat HIV.)
I didn’t realize at one point that my life would be ruled by a routine schedule for the coming days. My breakfast would be brought at a certain time along with a pack of different medicines that I had to take by 8am. Lunch would later follow along with a tablet that would be given to me in advance since I had to take it by 2pm.
Dinner would be served around 6pm along with the medicine that I had to drink at 8pm. I knew what times of the day and night someone would drop by to take my blood oxygen levels, temperature and blood pressure.
It became no longer inconvenient to be woken up past midnight because blood had to be taken from me or because someone had to measure my vitals and ask how often had I urinated or taken a poop. This schedule of activities became my new normal and daily routine.
One of the hardest things that I had to deal with during my hospital stay was the insomnia and the silence. I would spend the day resting. I would end up being too well-rested in the evening to fall asleep. I kept the bathroom light on and the door slightly ajar to act as a nightlight. It became tiresome staring in to the darkness waiting for sleep to come.
The silence at the hospital was not deafening. It allowed me to hear more during the night. I could hear a motorcycle travelling along the road outside my window. I could hear cicadas. I could hear the nurses outside in the corridor.
I could hear sounds that I didn’t want to hear. I heard someone coughing loudly as I lay down in bed. I heard what sounded like someone trying to get air into their lungs.
I developed a fever twice either because my body was reacting to my IV swollen hands and arm or it was fighting the virus. I would go sleep and feel cold. The chills made my body convulse in an effort to keep warm. A fever would set in and I would have to dip into the supply of paracetamol by my bedside to help cope with the fever. The fever would usually break after a few hours.
There were a couple of times the IV was left out long enough for me to take a bath. Eventually, I learned how to take off my shirt, take a bath, change into a fresh set of clothes even with the IV attached.
I didn’t think that I would have diarrhea for three weeks straight from my first ER visit. I lost 12 pounds during the first three days. I would lose 5 pounds a week during the succeeding two weeks.
My doctor had taken note of my weight loss. I asked him what was causing my diarrhea not to abate. He said that it was a combination of the virus, the medicines that I was taking and the fact that I wasn’t used to the hospital food.
One thing I became cognizant of very quickly was that I was staying in an isolation wing. There was a strict schedule when people when allowed to enter my room.
I once asked for my bed sheets to be changed. It was an hour before a male nurse came to change them. He apologized about the delay. I told him that it had been explained to me and I understood that they could only come to my room at certain hours. I thanked him for changing my sheets and told him that his safety was more important than my bed sheets.
(The same male nurse also explained to me that one reason why they couldn’t go to a patient as quickly as possible was because they would be at the delivery area waiting for their PPEs to be unloaded.)
The hospital staff would change PPEs several times during my stay. Old ones would be disposed off and everyone would switch to wearing a new set of PPEs. I think that the most difficult part of the PPE to wear would be the plastic face shield. You would see fogging and moisture develop on it as the hospital staff did their job.
One nurse was wearing glasses which was fogged along with her face shield. She had trouble seeing as she was trying to insert a needle into my hand. She brought my hand closer to my eyes, pointed to a spot and asked if I saw a vein where she was pointing. I put on my glasses, looked at where she was pointing and informed her that I was just as blind. She did manage to find the vein.
You would have to admire the hospital staff at Qualimed for their empathy. A male nurse kept checking on me one evening as I was coping with a fever. The nurses noticed that I kept on asking for an extra bottle of water with my meals because I was trying to cope with the dehydration due to the diarrhea. They would soon bring extra bottles with my meals without my having to ask for it.
One male nurse suggested that I buy big bottle of water and have it brought to me by a relative since my extra bottles of water would end up as an extra cost on my hospital bill.
A female nurse told me that the following day was her day off and offered to buy for me what I needed. She purchased for me a 6-liter bottle of mineral water, fabric conditioner and laundry detergent. It made me very happy to be able to do my own laundry. I was going to run out of clothes to wear. I underestimated how long I would have to stay at the hospital.
The bathroom sink would become my laundry area and the shower curtain rod would become the drying area.
It would take time for each swab test result to come back. I would openly curse all the government officials and their respective family members who all essentially cut in line to be tested delaying every else who needed testing.
My first swab test result came back after seven days. It was positive for Covid-19 as expected. My doctor did a good job of softening the blow. The second one also came back positive. I knew that I needed two negative results in order to be released from the hospital.
I told one of my brothers-in-law that I basically had an unlimited number of tries to get at least one negative swab test result.
Finally, the third swab result came back as negative. I started to get my hopes up.
A fourth swab test was taken on April 1 or April Fool’s Day. I didn’t want to think of it was a bad omen.
I saw a strange sight a few days later. My doctor and two nurses walked into my room with their PPE headgear off. It took me a few seconds to realize that the April 1 swab result had come back negative as well. I was congratulated by Dr. Pasayan and the nurses, photos were taken and I told Dr. Pasayan that I would honor my promise to him.
I had promised that after my release from the hospital, the mandatory 2 weeks of self-isolation and the lifting of the ECQ, that I would go back to Qualimed and take formal photos of him and the hospital staff that took very good care of me.
I am sincerely looking forward to keeping that promise after spending 18 days under their care.
Shared with permission from his Facebook post.